Inomyalgia is a term that has gained more attention in recent years, especially among people dealing with chronic pain that doesn’t go away despite rest or routine treatments. If you’ve ever felt deep, persistent muscle pain that lingers for weeks or even months—without a clear injury or explanation—you might have stumbled across the word “inomyalgia” in health forums, wellness blogs, or even while speaking with a healthcare provider. While not yet widely classified in medical manuals, it is increasingly being used to describe a condition that affects thousands in silence.
This guide breaks down everything you need to know about inomyalgia in 2026. From its symptoms and causes to available treatments and self-care strategies, you’ll find accurate and up-to-date information written in a way that’s clear, supportive, and grounded in real insight.
Quick Bio Information
| Key Fact | Details |
|---|---|
| Name | Inomyalgia |
| Definition | Chronic, deep muscle pain lasting for weeks/months |
| Type | Musculoskeletal condition |
| Common Symptoms | Pain, stiffness, fatigue, brain fog |
| Primary Affected Areas | Localized or regional muscles |
| Duration | Long-lasting (weeks to months) |
| Visibility | Often invisible externally |
| Risk Factors | Stress, nutrient deficiencies, poor posture |
| Diagnosis | By symptom pattern and exclusion |
| Related Conditions | Fibromyalgia, CFS, myofascial pain |
| Typical Age Group | Adults (20s–60s), but not exclusive |
| Mental Health Link | Commonly associated with anxiety, depression |
| Current Recognition | Emerging, gaining awareness |
| Treatments | Medical, holistic, and lifestyle-based |
| Prognosis | Manageable with long-term care |
What Is Inomyalgia? A Simple, Clear Definition
Inomyalgia refers to a persistent type of muscle pain that is not caused by an injury or temporary overuse. It is chronic, often appearing in specific regions of the body, and can be incredibly disruptive to daily life. Unlike regular muscle soreness from a workout, inomyalgia pain sticks around. It may feel dull, aching, or throbbing and doesn’t resolve with sleep, rest, or typical painkillers.
The name itself combines “ino” (meaning muscle tissue or connective tissue) and “myalgia” (muscle pain). This reflects its nature: a deep, tissue-level discomfort rather than surface-level soreness. In many cases, people with inomyalgia appear healthy on the outside but live with pain that affects their ability to work, exercise, or even rest comfortably.
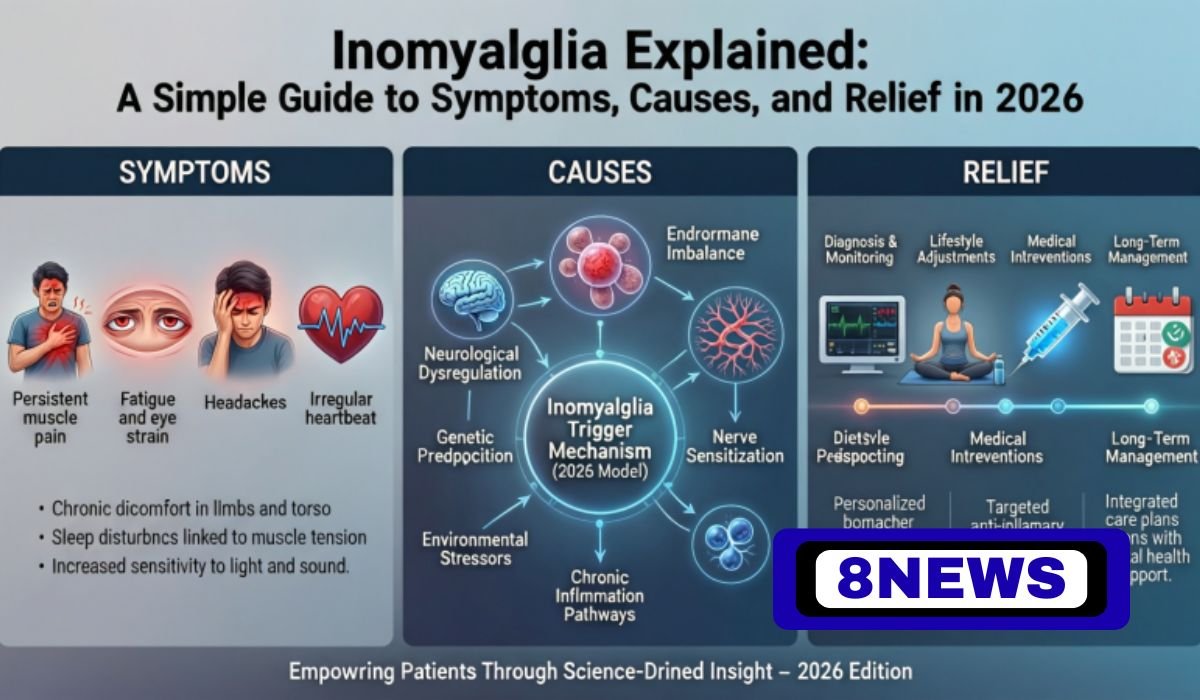
What Causes Inomyalgia? A Look At The Main Triggers
Inomyalgia isn’t typically caused by one single issue. Instead, it often develops from a mix of internal and external factors that wear down the body’s muscular and nervous systems. Genetics may play a role, especially for those with a family history of chronic pain. Other times, it’s environmental—stress, inactivity, or nutritional deficiencies can all contribute.
When you don’t get enough sleep or your body lacks important vitamins like magnesium, B12, or vitamin D, your muscles can’t repair themselves properly. Hormonal shifts, such as changes in cortisol or serotonin levels, can amplify how your body experiences pain. Chronic tension from stress or even poor posture at work can quietly build up until your muscles are in a state of constant strain.
Inomyalgia is also being studied in relation to viral or autoimmune reactions. Some people notice symptoms flaring after a bout of illness, suggesting immune involvement.
Common Symptoms Of Inomyalgia: How It Feels In Daily Life
The most noticeable symptom of inomyalgia is long-lasting muscle pain that refuses to go away. This pain isn’t necessarily sharp. Instead, it’s usually described as aching, heavy, or sore—often concentrated in the neck, shoulders, lower back, or hips. It can be one-sided or affect multiple muscle groups at once.
Morning stiffness is especially common. Many people say they wake up feeling as if their body is stuck in place or that it takes hours to loosen up. Fatigue is another hallmark symptom. Even after a full night’s sleep, energy levels may feel depleted. Trouble concentrating, often referred to as “brain fog,” can make work or communication difficult.
Because this condition isn’t visible from the outside, people with inomyalgia often feel misunderstood or even judged for “looking fine” while battling deep discomfort every day.
Inomyalgia Vs. Fibromyalgia: Key Differences You Should Know
It’s easy to confuse inomyalgia with fibromyalgia, but there are some key differences. Fibromyalgia usually causes widespread pain across the body and is commonly associated with heightened nerve sensitivity and cognitive issues like memory lapses. It also has clearly defined clinical criteria that doctors can follow for diagnosis.
Inomyalgia, by contrast, is typically more localized. You might feel pain in specific muscles or body regions, such as your upper back or thighs. While brain fog and fatigue can occur, they are usually less severe. Inomyalgia is also newer in terms of terminology and not as widely accepted yet in formal medical systems, though it’s gaining recognition through patient experiences and recent research.
Understanding the distinction is important, because treatment strategies may differ based on symptom patterns.
How Doctors Diagnose Inomyalgia
Since there is no blood test or imaging scan that confirms inomyalgia outright, doctors rely heavily on symptoms, physical examinations, and ruling out other possibilities. They may begin by asking how long the pain has lasted, where it is located, and whether it changes with activity or rest.
Medical providers often check for tender points and muscle stiffness. You might be asked about your energy levels, sleep habits, and mental well-being. Blood work can help rule out conditions like thyroid dysfunction or vitamin deficiencies, while MRIs or X-rays may be used to eliminate injury-related causes.
Doctors might recommend that patients keep a journal to track when pain flares up, what triggers it, and how it responds to treatments. This record becomes a valuable tool in creating a personalized care plan.
Best Medical Treatments For Inomyalgia In 2026
Managing inomyalgia often begins with addressing the pain itself. Doctors may recommend over-the-counter options like ibuprofen or acetaminophen, especially during flare-ups. In some cases, low-dose antidepressants such as SSRIs or SNRIs are prescribed. These don’t just help mood—they also affect how the brain interprets pain and can improve sleep.
If nerve-related pain is involved, medications like pregabalin or gabapentin may be introduced. Additionally, blood tests might reveal deficiencies in vitamin D, magnesium, or B12, and supplementation is prescribed accordingly.
While medications can be helpful, they are usually part of a broader treatment plan. The goal is not just to mask symptoms, but to support the body’s natural ability to heal and regulate pain signals.
Holistic And Lifestyle Relief Options Backed By Real Benefits
In 2026, more people are turning to lifestyle changes and holistic care to manage chronic conditions like inomyalgia. Gentle movement is one of the most powerful tools available. Stretching, yoga, water aerobics, or walking can reduce stiffness and help retrain muscles without overloading them.
Physical therapy is often recommended to target muscle imbalances, improve posture, and develop a pain-friendly exercise plan. Diet is also crucial—anti-inflammatory foods like berries, leafy greens, fish, and olive oil can help lower pain levels over time.
Many patients find relief through alternative therapies such as acupuncture, massage, or cupping. While not a cure, these methods can improve circulation and relax muscle tissue. Stress management techniques like meditation, deep breathing, and mindfulness are also essential tools in breaking the pain–stress cycle.
Living With Inomyalgia: Daily Tips That Make A Big Difference
Creating a routine that supports your body’s healing is one of the most effective ways to live well with inomyalgia. Start the day with gentle stretching and avoid jumping straight into strenuous tasks. Use ergonomic chairs or standing desks to reduce strain while working.
It’s important not to overexert yourself on good days. Pacing is key—alternate between activity and rest to prevent flare-ups. Keeping track of triggers like weather changes, sleep disruptions, or emotional stress can help you prepare or respond better next time.
Support matters too. Talking openly with friends or joining online communities can reduce the emotional weight of the condition. You’re not alone, and many people are walking a similar path.
Inomyalgia And Mental Health: The Hidden Emotional Burden
Chronic pain doesn’t just affect your muscles—it impacts your mood, self-esteem, and relationships. One of the hardest parts about inomyalgia is how invisible it is. When others can’t see your pain, you may feel isolated or invalidated. This can lead to anxiety, depression, or withdrawal.
Many people with inomyalgia say they feel frustrated at not being believed or supported. It’s important to recognize these emotional reactions and treat them with the same seriousness as physical symptoms. Talking with a mental health professional, joining support groups, or engaging in therapy like CBT can help rebuild resilience.
In 2026, more healthcare providers are acknowledging the strong link between chronic pain and mental health, leading to more holistic, person-centered care.
Can Inomyalgia Be Prevented? What Science Suggests For 2026
While not every case of inomyalgia can be prevented, adopting healthy habits can significantly lower your risk or delay its onset. Managing daily stress through activities like journaling, tai chi, or mindfulness practice keeps your nervous system from staying in a chronic state of alertness.
Sleep is also a major factor. Creating a bedtime routine, avoiding screens before bed, and maintaining a dark, quiet sleeping environment helps your muscles recover and regulate hormones. Staying physically active, even with light movements, maintains healthy circulation and muscle tone.
Nutrition matters—make sure to eat balanced meals rich in vitamins and minerals. If you have a family history of chronic pain, consider early interventions like physical therapy, ergonomic adjustments, or routine blood checks to catch imbalances before they manifest as symptoms.
When Should You See A Doctor? Warning Signs You Should Not Ignore
If your muscle pain lasts longer than a few weeks, is getting worse, or interferes with your ability to work, sleep, or concentrate, it’s time to talk to a doctor. Don’t wait for symptoms to become unbearable—early attention makes treatment easier and more effective.
Other red flags include swelling, unexplained weight loss, fevers, or pain that wakes you up at night. If your discomfort is accompanied by severe fatigue or mood changes, these could be signs of overlapping conditions that need medical attention.
It’s also important to seek help if you feel emotionally overwhelmed. Healthcare is not just for fixing what’s broken—it’s also for preventing burnout and maintaining wellness.
The Future Of Inomyalgia Research: What Experts Are Studying Next
Inomyalgia is finally entering the research spotlight. Scientists are studying how chronic inflammation affects muscle tissue and what role pain signaling pathways play in keeping the nervous system in a heightened state. Some studies are investigating whether genetic markers could predict vulnerability to chronic muscle conditions.
There’s also growing interest in how gut health and immune system balance affect muscular inflammation. Clinical trials are exploring new drug therapies that target deep tissue sensitivity, while others focus on how lifestyle-based interventions may slow or reverse symptoms.
As the scientific world catches up to patient experience, the hope is that inomyalgia will receive formal recognition, clearer diagnostic criteria, and even more effective treatments.
Conclusion
Inomyalgia is more than just lingering muscle pain—it’s a life-altering condition that affects how people move, think, and feel. The good news is that with growing awareness and a combination of medical and holistic care, it can be managed. Understanding what causes the condition, recognizing the symptoms early, and creating a personalized care plan are the first steps toward long-term relief.
If you or someone you know is experiencing persistent, unexplained muscle pain, don’t brush it off. Reach out, speak with a healthcare provider, and start tracking your symptoms. Knowledge is the key to healing, and you don’t have to face this condition alone.
FAQs About Inomyalgia
What Is Inomyalgia?
Inomyalgia is a term used to describe long-term muscle pain that affects specific parts of the body. It differs from regular soreness because it doesn’t go away easily and often comes with fatigue and stiffness.
How Is Inomyalgia Diagnosed?
There is no specific test for inomyalgia. Doctors diagnose it by examining symptoms, ruling out other conditions, and sometimes using blood work or imaging to confirm there is no injury or disease.
Is Inomyalgia The Same As Fibromyalgia?
No. Fibromyalgia causes widespread pain, while inomyalgia usually affects localized areas. Fibromyalgia also includes severe fatigue and brain fog more consistently. Inomyalgia is still gaining medical recognition.
What Causes Inomyalgia?
Possible causes include chronic stress, poor posture, lack of vitamins like D or magnesium, hormonal imbalance, or even past viral infections. It usually results from multiple factors, not just one.
Can Inomyalgia Go Away On Its Own?
It can improve with treatment and lifestyle changes, but it often requires active management. Without addressing the root causes, symptoms may return or worsen.
Is Inomyalgia A Mental Condition?
No, it is a physical condition with emotional impacts. While mental health is affected by chronic pain, inomyalgia is based in muscular and possibly neurological dysfunction.
What Are The Best Treatments For Inomyalgia?
Treatment includes pain relief medication, supplements (if needed), physical therapy, exercise, and stress-reduction strategies like meditation and massage. A personalized care plan works best.
Can You Prevent Inomyalgia?
While not all cases can be avoided, maintaining a healthy lifestyle—good sleep, low stress, proper nutrition, and regular movement—can reduce your risk.
People Also Read: Ark Augmented Reality: The Technology Changing How We See the World